If you don’t ask, you don’t get!

Few would disagree that recent decades have witnessed massive advances in the care offered to some people with bleeding disorders. For many bleeding disorders, the treatment landscape continues to evolve; for others the struggle to be recognised continues, especially among women.
Delegates attending The Haemophilia Society AGM and Members Conference in Liverpool this weekend heard about many of the recent advances in treatment and care, giving them a chance to reflect on the potential for their lives and those of their families/carers. Assuming, that is, they are given the opportunity to access these new treatments. The extended half-life factor concentrates were introduced a few years ago, offering the promise of either less frequent dosing or higher trough levels. Yet patients continue to report being refused the opportunity to switch to EHLs, or being switched from EHLs to standard half-life factors. This is, of course, driven by cost and the limitations placed on clinicians by the commissioning process.
Yet no such problems in Ireland, where most patients are now on EHL products. In his presentation, health economist Jamie O’Hara noted that in 2002, Ireland and Belgium had similar levels of factor VIII per head utilisation but Ireland was paying more. Successful advocacy by the Irish Haemophilia Society meant that by 2014, the country’s rate of FVIII utilisation per head was ahead of Belgium, yet it paid considerably less than Belgium. Jamie emphasised that this was driven, in part, by the fact that Ireland was able to use hard data to support its advocacy efforts, and he urged all delegates to complete their Haemtrack records.
Jamie’s session was entitled “The Disability Paradox”, and he showed how people with haemophilia often perceived themselves to have a good quality of life, despite living with pain and joint damage. He encouraged people to complete the outcomes and quality of life questionnaires that they were often given in clinics, as these can support advocacy for the whole community.
Most importantly he urged the audience to ensure they were well informed so they could advocate for themselves. Patient associations can play a major role in supporting their members to be informed of new developments, as can healthcare professionals (HCPs) in their everyday engagements with patients. At a time when the language of haemophilia is changing rapidly staying informed and up to date isn’t always easy…(even for HCPs!)
After years of thinking “factor”, remembering to check understanding when talking about monoclonal antibodies, viral vectors or antithrombin is really important for healthcare professionals and patient associations alike.

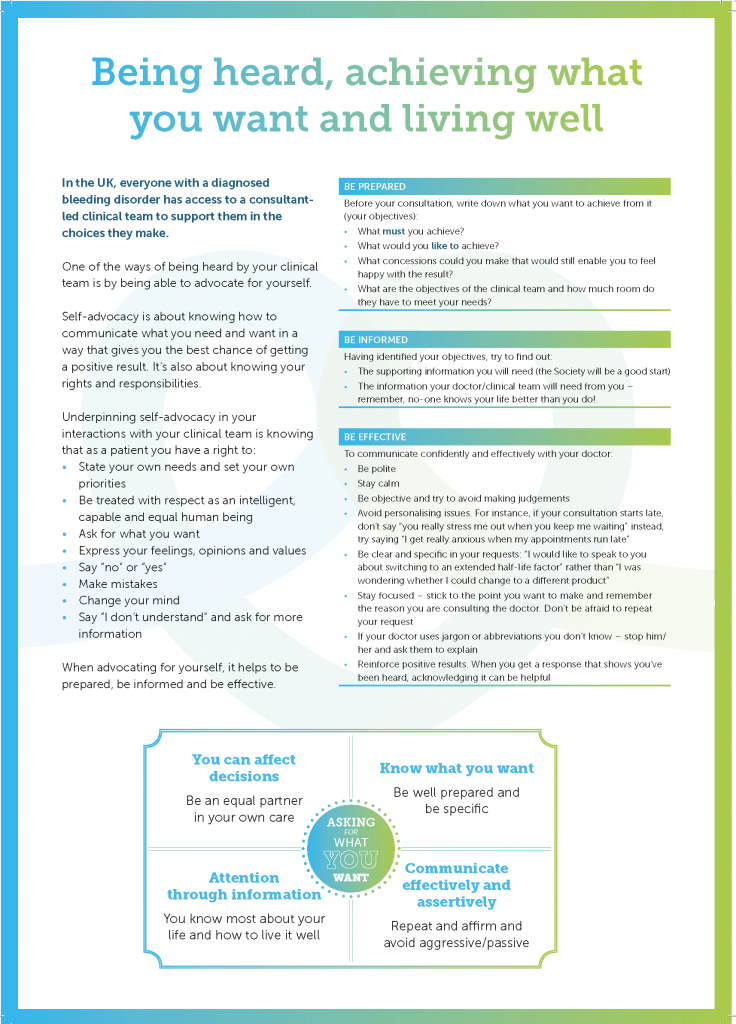
Haemnet opened the conference with a session on “Being Heard and Getting What You Want from a Consultation.” As part of our session, we asked delegates what would make a consultation successful. Aside from “treatment” (no surprise there), the words that featured loudly were “informative”, “listening”, and “understanding” – as you can see in our word cloud.
But how do you make sure you are heard in your everyday consultation? How do you get the best out of them? And how do you make sure that you don’t leave thinking “If only I had asked…” Or worse still, that that there has been no engagement at all. We heard from one parent who’d recently been in a consultation where the doctor had never looked up from his computer screen to address her son directly. Fortunately, this mother told him in no uncertain terms that this was not acceptable!
Consultations that are collaborative conversations are the ones where patients feel comfortable talking about their lives and their health, and what’s important to them; and where healthcare professionals can contribute their expertise to support patients in living their lives. How we as individuals approach these conversations can have a huge influence on what we get out of them. Our beliefs about what we can achieve in any given situation influence our behaviour and can influence the behaviours of others. As a patient, going in to a consultation and expecting to be heard goes a long way towards being heard; going in well prepared and knowing what you want changes the conversation and improves the chances that you’ll come out with a positive result.
Researchers have identified five patient types:
- Passive-dependent – those of us who believe the doctor know best.
- Intellectual-researcher – those who are willing to research their health conditions online or in journals and expect to participate in decision-making.
- Independent-sceptical – those who are sceptical about any advice from experts.
- Expedient-flexible – people who take the view that any doctor will do, they’re all the same.
- Open-minded-exploring – those of us who see health care as a partnership between doctor and patient.
When asked to describe themselves in relation to these types, it was great to see that most THS members in the room were prepared to advocate for themselves and the people for whom they care. The real challenge for all patient associations is supporting the wider population to be as actively engaged in their care, and for the NHS to support their practitioners to be positively responsive.
Sadly, this doesn’t happen in all consultations. Persistence from us all – whether we are patients, family members, carers or HCPs – can lead to changes in our experience of consultations. You must become the best advocate for yourself with the aim of communicating “what you want in a way that gives us the best chance of getting a positive outcome.”
You can use the following link to download our crib sheet on “Being heard, achieving what you want and living well.”