
Survey Results
Online survey promoted to people with a bleeding disorder, their families and health
professionals in the UK
(via social media and other routes)
302
Completed responses
(from people with a bleeding disorder or their
representative)
17 minutes - mean time for survey completion
Age and diagnosis
Respondents included:
People with a bleeding disorder
Carriers
Parents
Partners &
2 siblings
Age distribution of people
with bleeding disorders
Age distribution was fairly evenly distributed between three groups:
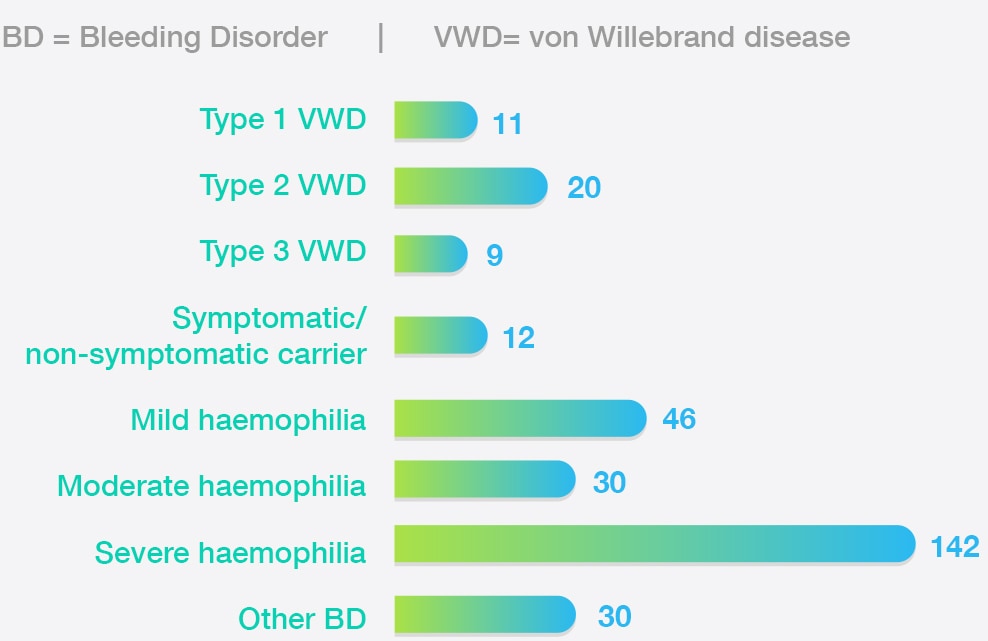
Reported diagnosis
300 respondents reported a diagnosis
Treatment centres
Journey times / Frequency of visits
301respondents stated they were registered at a treatment centre in the uk
Their journey times:
30 - 60 minutes
1 - 2 Hours
Less than 30 minutes
Over 2 hours
'Long travel to get there, in a lot of cases a phone call would achieve the same end.'
Frequency of routine visits to treatment centre, pre - pandemic
Before the pandemic most people visited their centre (annually):
Quality of Care
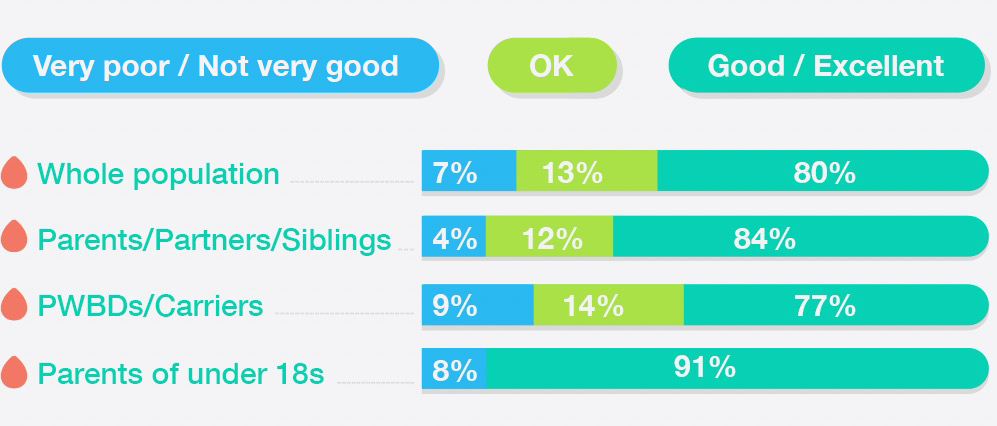
Most respondents rated the quality of care they received as good or excellent. A notable minority rating their care as OK or very poor/not very good.
Some of the frustrations expressed involved:
Positive ratings were highest among parents of under 18s and lower among people with a rare bleeding disorder or diagnosed as a carrier
'Friendly, responsive, knowledgeable health care professionals who support my son and us very well.'
'Care is hit and miss, sometimes it is outstanding; other times I have not received contact back.'
'It falls short of excellent as there is not access to physiotherapy services except in extreme circumstances. I feel others would benefit from regular joint assessment and advice on appropriate exercise programmes compatible with my physical condition.'
How
respondents rated
quality of care
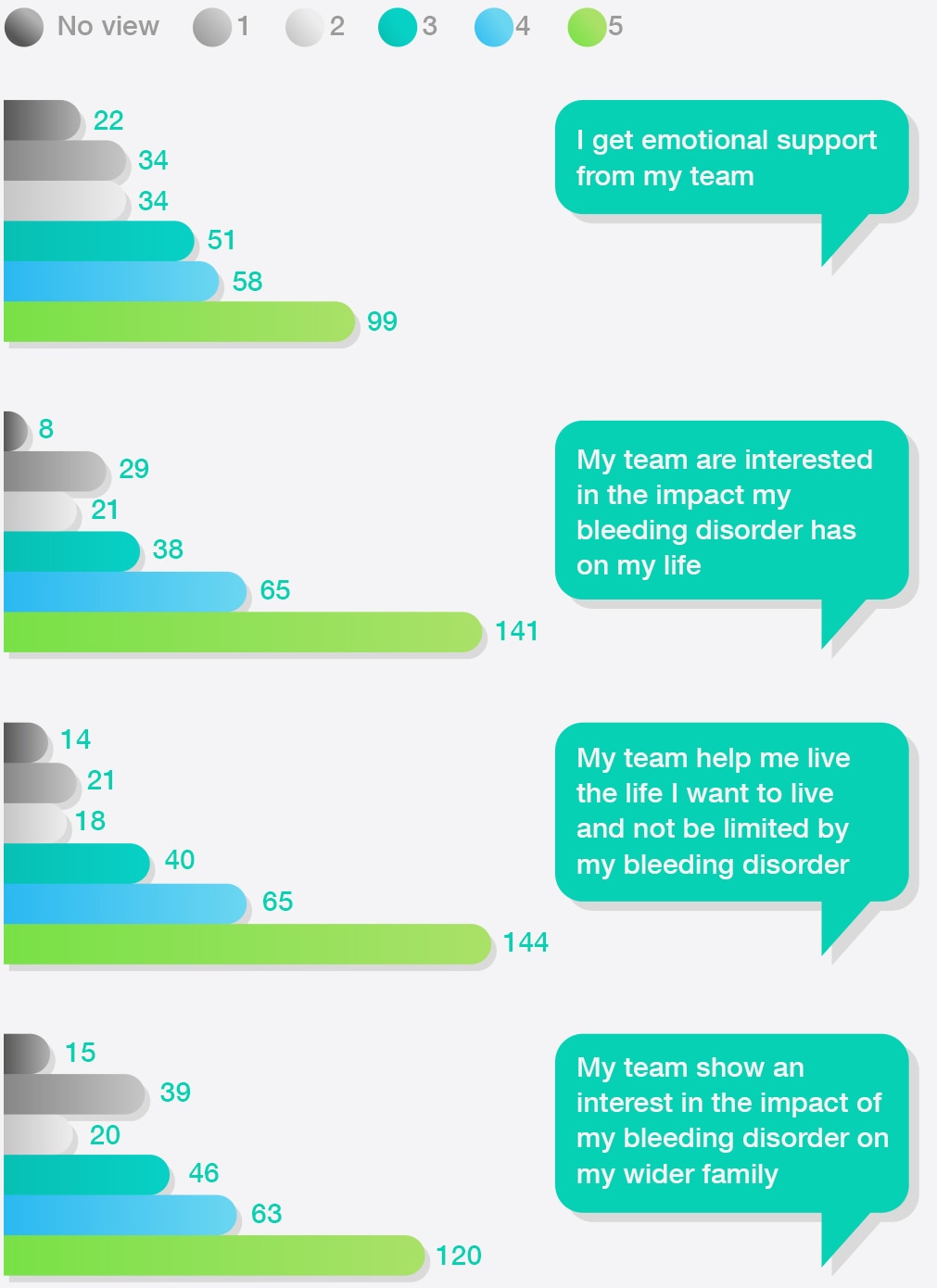
Support from Multidisciplinary Teams
2/3 Agreed or strongly agreed their care team:
- Are interested in the personal impact of their bleeding disorder
- Support them to live the life they want
52% Agreed or strongly agreed their care team provide emotional support
23% Disagreed or strongly disagreed their care team provide emotional support
'I value the personal effort each member of staff puts into knowing their patients and listening to us. Treatment at the... CCC (comprehensive care centre) is an inclusive team effort where everyone, including the patient, is as important as everyone else.'
'Frustration that they are unable to provide or fund the psychological support that will be needed when times are difficult.'
How
respondents rated support
from the multidisciplinary team
'I've had many situations that involved making new decisions about my healthcare and I've always received good advice that has benefited me.'
'I find it hard to approach the centre and if I do it is because I genuinely feel I need help and assistance but when that isn’t provided , I lack confidence to contact them in the future.'
'Most of my reasons for treatment are ‘self-inflicted’ - i.e. due to an overactive lifestyle but they do not judge or lecture me. Also the friendliness and the speed of being seen.'
Other medical services
Most did not agree that other non-specialist health professionals understood their bleeding disorder with around:
- 50% felt this was the case for GPs and A&E consultants in accident and emergency
- 40% felt this was the case for paramedics
Ratings of other medical services were consistent among all respondent groups
'.. the ambulance service can now only take you to the nearest hospital with A&E. Sadly those hospitals cannot cope with haemophilia.’
'My local A&E has no understanding of haemophilia and on 2 occasions over the last 3 years has failed to consult my haemophilia centre when dealing with me in an emergency situation.'
'More communication is needed between the GP and the treatment centre'
How
respondents rated
non-specialist health professionals’
understanding of their
bleeding disorder

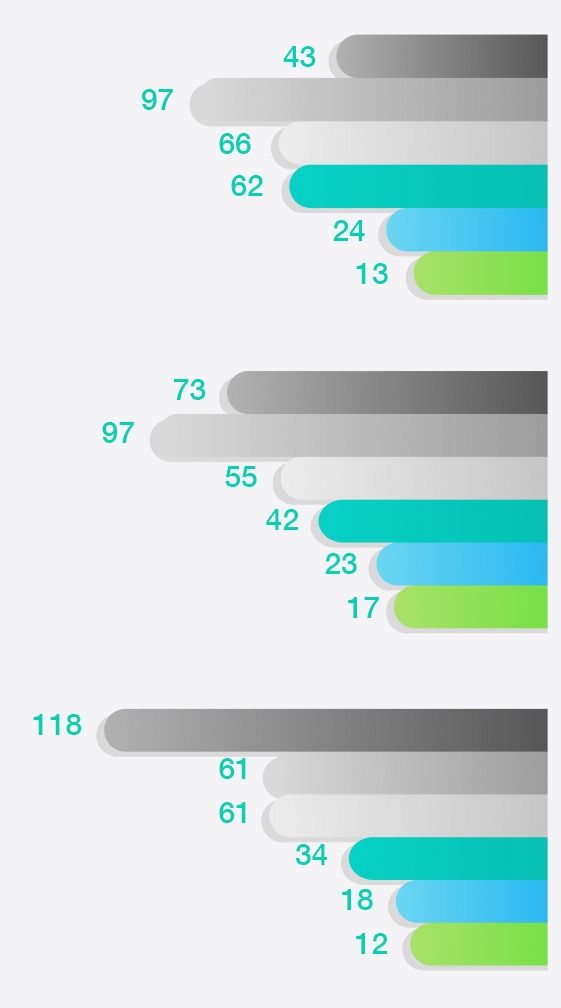
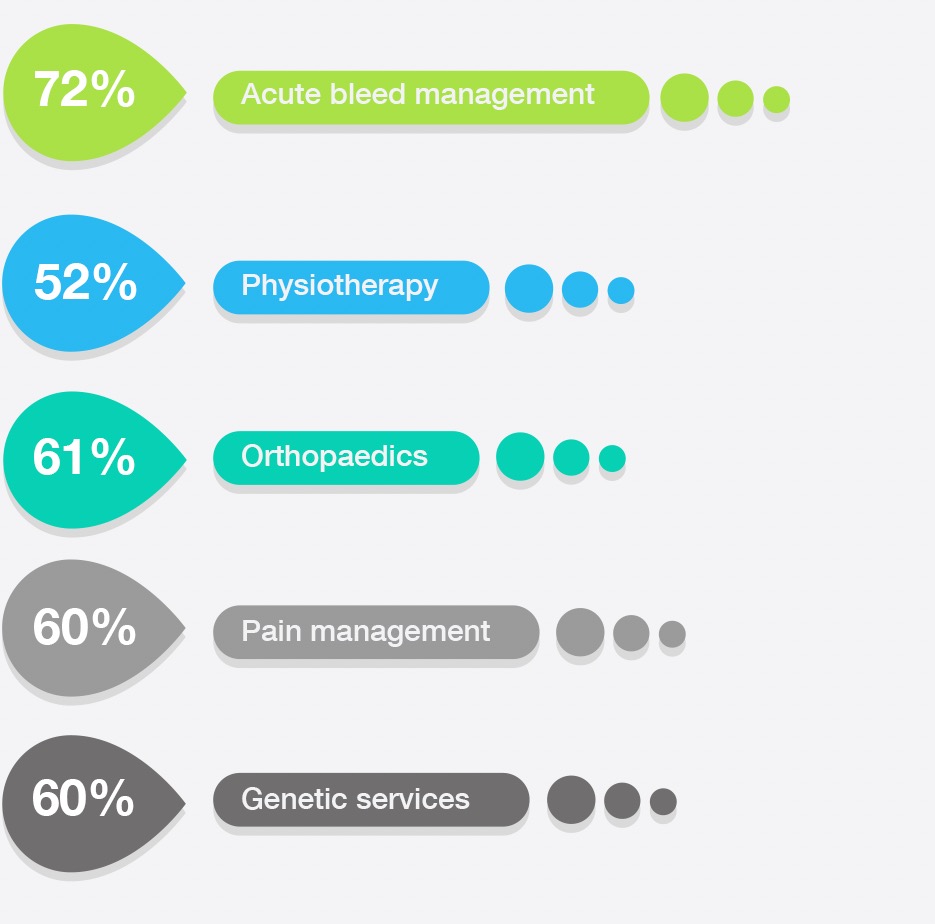
Services Used
Services rated
good or excellent
by most respondents
Ratings of services used by respondents were mixed:
'The services provided by the nurses, doctors and physios are
excellent.
... Unfortunately, though, there is no social worker in place or dental team, even though this
is a
comprehensive care
centre.'
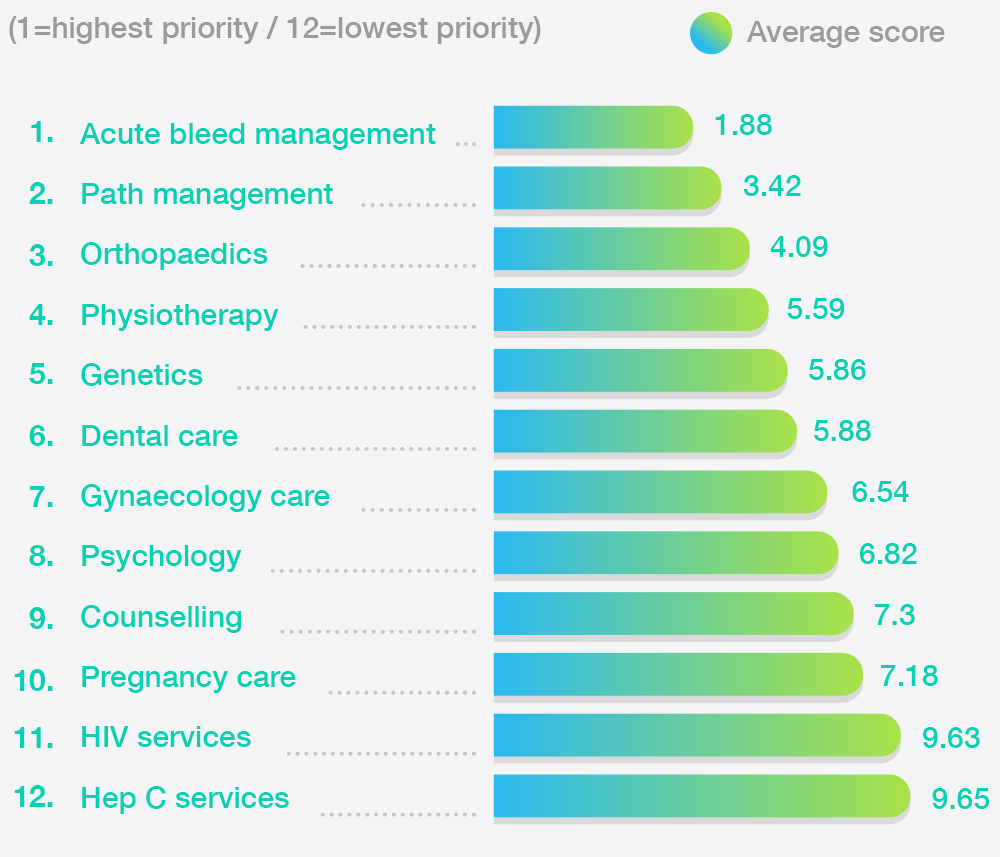
Respondents'
average rating of
priority for integral services
When rating the priority for access to services, management of acute bleeds, pain management and orthopaedics were rated highest priority.
Post-COVID Preferences
55% of respondents said there had been changes in their care due to the COVID-19 pandemic. Alternatives to face-to-face contact were generally recieved positively, but for some they reinforced a sense of disconnect with the care team.
Preferences for how treatement centres should keep in touch included digital and non-digital options:
'I’m just having phone call appointments and management and I don’t like it.'
'I had blood tests done last month in my local surgery and a telephone appointment. This is a great idea as it reduces the need for travel and the risk of visiting the hospital whilst Covid is still prevalent.'
'Telephone-based appointments has its upsides and downsides... I've also noticed a difference between those centres who use video and those who only use phone. The use of video feels more personable .'
Conclusion
The Phoenix survey shows that most respondents value the services provided by their treatment centres but a minority, sometimes large, rated some aspects of the services as poor or absent.
This is consistent with the findings of the West Midlands Quality Review Service peer review process commissioned by the UKHCDO.
Care beyond specialist centres, especially that provided through A&E and by GPs, is a continuing concern.
Further exploration of how treatment centres reorganised the services during COVID-19, and the impact of this on people with bleeding disorders, could help to ensure that:
- The changes that work well become standard practice
- These changes support NHS aims for personalised service provision
Providing greater support for treatment centres to share effective practice and resources would contribute to delivery of a more uniformly high standard of care.
